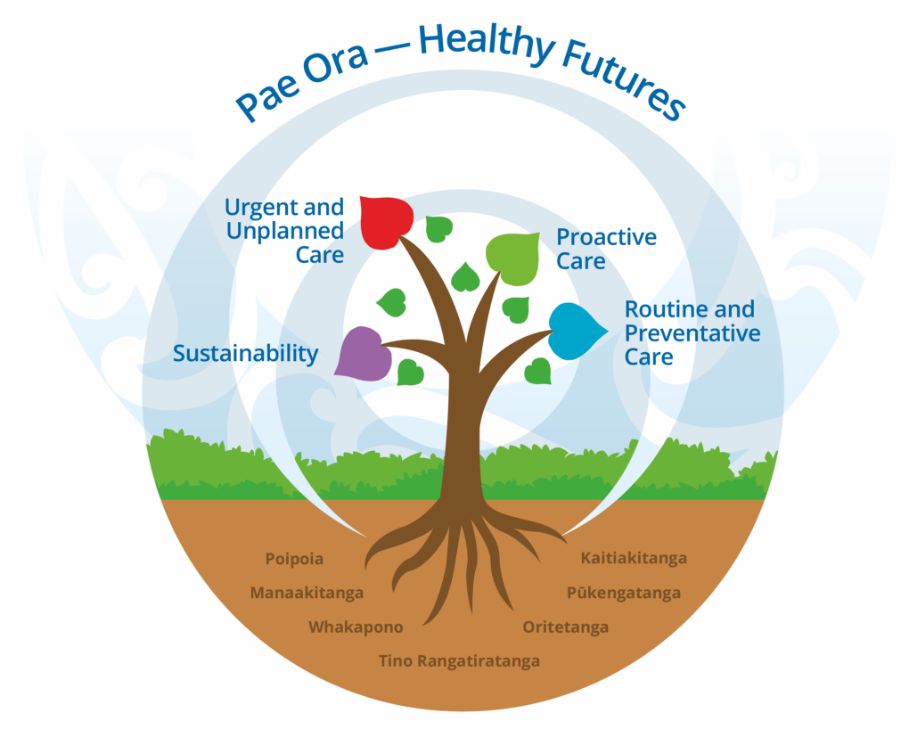
The Enhanced Model of Care is a practical whānau-centric approach to modernisation of primary care, leading to a better patient and staff experience enhanced quality of care, and improved sustainability.
We continually review and refine the Health Care Home Model of Care to ensure that it improves patient/whānau care and health outcomes.
Practices may choose to implement some or all of the characteristics, by choosing aspects that fit the needs of its community/whānau. This is not a one size fits all model of care but one that is flexible and adaptive.
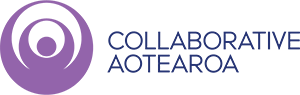
The HCH MoC incorporates whakawhanaungatanga (creating a relational model) in the delivery of care. Relationship centred care creates better health outcomes for our whānau. This can be as simple as ensuring that practice information resonates with people in terms of language and visual presentation or enhancing the cultural skills and competencies of staff, including understanding the unconscious bias inherent in many public services.
‘If the model delivers for Māori, it will deliver for most of our priority communities and, ultimately, for all New Zealanders.’