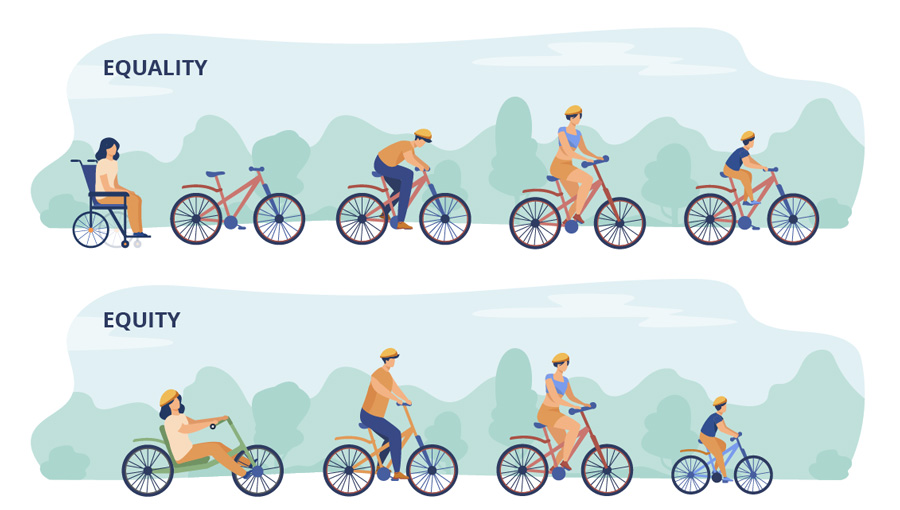
Collaborative Aotearoa aims to provide every New Zealander with equitable access to health and wellbeing services across Aotearoa.
We are particularly focused on equitable health and wellbeing outcomes for Māori groups who have previously faced bias when accessing healthcare resources. We are supported by, and continue to embed, Māori input within our practices. It is important to us to strive for health equity to ensure your whānau feel confident and assured when accessing services.
Our commitment in reviewing and enhancing the HCH model of care has been to ensure that it improves patient/whānau care and hauora outcomes. As the model grows and matures, we constantly challenge its contribution to improvement in equity of access and outcomes for those communities in need of additional support, particularly Māori. If the HCH model delivers for Māori, it will deliver for most of our priority communities and ultimately lead to better outcomes for everyone.
We believe all patients should receive excellent health and wellbeing care regardless of their socio-economic, demographic or geographic status.